Immune System Overview for Nursing Students (Structure and Function)
Types of immune responses: Innate and adaptive, humoral vs. cell-mediated
Innate vs. adaptive immunity. Humoral adaptive immunity vs. cell-mediated adaptive immunity.
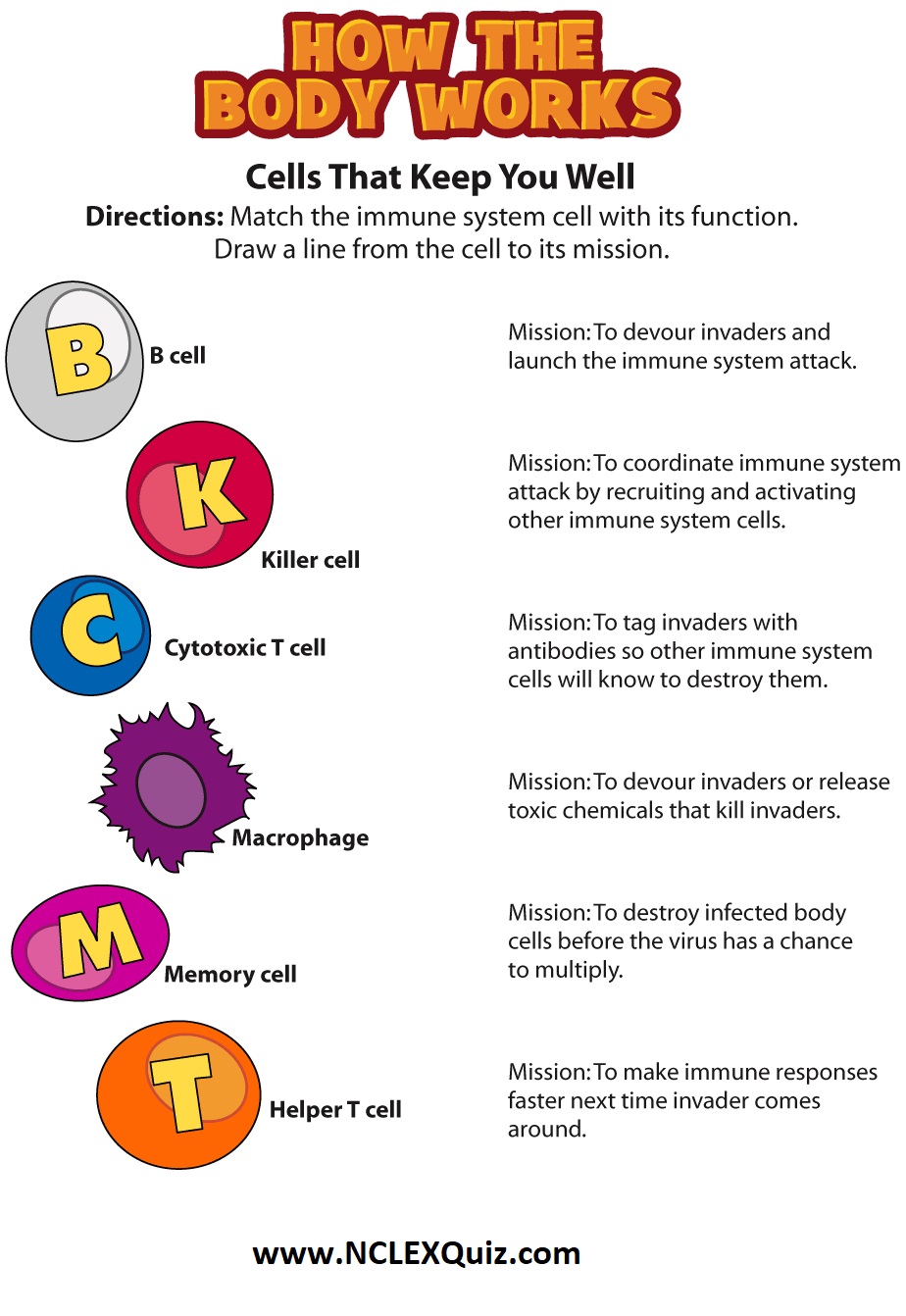
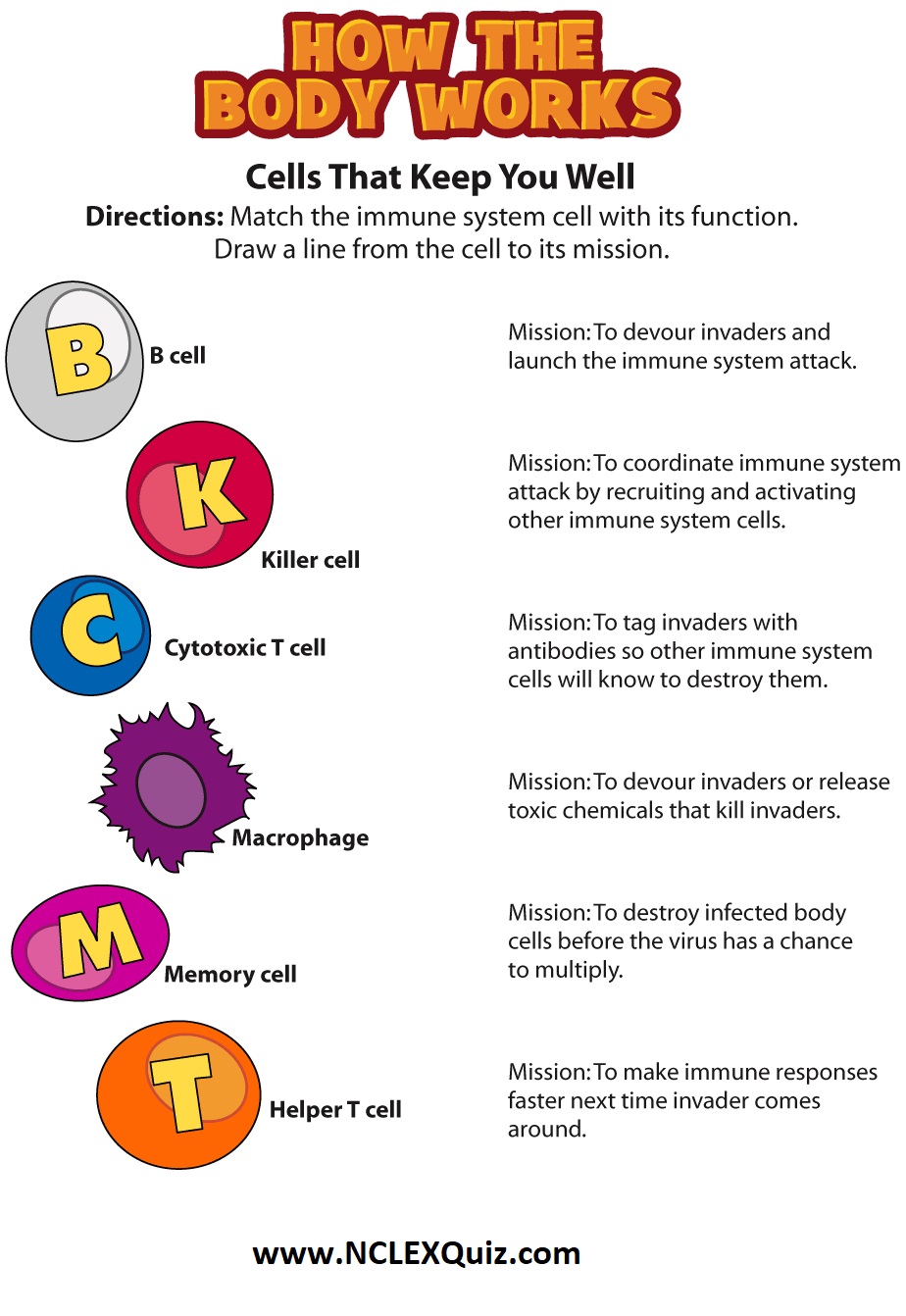
Do you know your immune system? Label the parts of the system that keeps you well.
What is the immune system?
The immune system protects your child’s body from outside invaders, such as bacteria, viruses, fungi, and toxins (chemicals produced by microbes). It is made up of different organs, cells, and proteins that work together.
There are two main parts of the immune system:
1. The innate immune system, which you are born with.
2. The adaptive immune system, which you develop when your body is exposed to microbes or chemicals released by microbes.
These two immune systems work together.
The innate immune system
This is your child’s rapid response system. It patrols your child’s body and is the first to respond when it finds an invader. The innate immune system is inherited and is active from the moment your child is born. When this system recognizes an invader, it goes into action immediately. The cells of this immune system surround and engulf the invader. The invader is killed inside the immune system cells. These cells are called phagocytes.
The acquired immune system
The acquired immune system, with help from the innate system, produces cells (antibodies) to protect your body from a specific invader. These antibodies are developed by cells called B lymphocytes after the body has been exposed to the invader. The antibodies stay in your child’s body. It can take several days for antibodies to develop. But after the first exposure, the immune system will recognize the invader and defend against it. The acquired immune system changes throughout your child’s life. Immunizations train your child’s immune system to make antibodies to protect him or her from harmful diseases.
The cells of both parts of the immune system are made in various organs of the body, including:
Adenoids. Two glands located at the back of the nasal passage.
Bone marrow. The soft, spongy tissue found in bone cavities.
Lymph nodes. Small organs shaped like beans, which are located throughout the body and connect via the lymphatic vessels.
Lymphatic vessels. A network of channels throughout the body that carries lymphocytes to the lymphoid organs and bloodstream.
Peyer’s patches. Lymphoid tissue in the small intestine.
Spleen. A fist-sized organ located in the abdominal cavity.
Thymus. Two lobes that join in front of the trachea behind the breastbone.
Tonsils. Two oval masses in the back of the throat.